Fosfomycin is an antibiotic (discovered in 1969) that has been making a resurgence in popularity in the last few years due to its activity against both gram-positive and gram-negative bacteria. Currently, it is a treatment option for women with uncomplicated urinary tract infections with the benefit being that it can be given in a single oral dose. In this blog post, I will discuss the top 5 clinical pearls to know about fosfomycin.
Lots of Coverage
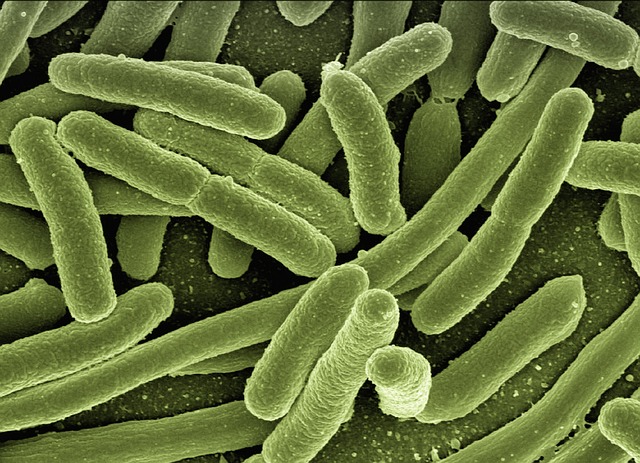
As stated previously, fosfomycin has activity against both gram-positive and negative bacteria, but more specifically, it has activity against Enterococcus spp. (which includes E. faecalis and E. faecium), Staphylococcus epidermidis, and S. aureus (both MSSA and MRSA). Activity against gram-negative bacteria includes E. coli, Klebsiella spp., Shigella spp., Salmonella spp., Serratia spp., Citrobacter spp., Enterobacter spp., and Proteus mirabilis. Fosfomycin is not active against anaerobes, Pseudomonas spp, Mycobacterium tuberculosis, Morganella morganii, and Acinetobacter spp.
Unique Mechanism
Fosfomycin is a bactericidal agent that works by inhibiting phosphoenolpyruvate transferase, the first enzyme used for the synthesis of peptidoglycan (a key molecule in cell wall construction). This subsequently inhibits biosynthesis of the bacterial cell wall.
UTI Treatment Only
Despite the wide spectrum of coverage that Fosfomycin provides, its only FDA-indicated use is for the treatment of uncomplicated urinary tract infections in women due to susceptible strains of E. coli and Enterococcus faecalis. Off-label usage includes infection caused by ESBL bacteria, dialysis-associated peritonitis, UTI with pregnancy, and prophylaxis for needle biopsy of the prostate. Fosfomycin is historically not recommended for the treatment of complicated UTI or pyelonephritis due to questions about limited renal penetration and a lack of randomized controlled trials. This is controversial with a somewhat recent retrospective study potentially indicating some success in treating pyelonephritis. Hopefully, we get stronger evidence to improve our confidence in whether this is appropriate or not.
C. Diff and Vaginitis
The most common side effects associated with Fosfomycin include diarrhea, nausea, and headache, but some more unique side effects can occur with this antibiotic. This includes vaginitis, dysmenorrhea, and rarely C. diff infections. Additionally, Fosfomycin can cause electrolyte imbalances such as hypernatremia and hypokalemia, however, this is associated mainly with the IV formulation.
One Dose is All It Takes
Fosfomycin’s recommended use in UTI treatment is with a single dose of oral granules, which are used by mixing the provided packet of medication into 3-4 oz of water and stirring to dissolve the granules. Repeat dosing of fosfomycin is generally not recommended as there is no observable additional benefit after the one dose and an increased rate of side effects. Other therapeutic alternatives should be chosen if the infection persists.
Are you seeing fosfomycin used in your practice?
Looking for more on UTIs? There’s a new drug that was recently approved. Here’s the rundown on pivmecillinam.
This article was written by PharmD Candidate Emma Carlberg in collaboration with Eric Christianson, PharmD, BCPS, BCGP
- 30 medication mistakes PDF
- 18+ Page Drug Interaction PDF
- 10 Commandments of Polypharmacy Webinar based on my experiences in clinical practice








0 Comments