In this case scenario, we discuss the interplay between prednisone in diabetes. Clinical situations like this are frequent in practice and prednisone can really mess up a patient’s well-controlled blood sugars (common board exam question). Here’s the situation.
LS is a 58 year old female with a history of severe rheumatoid arthritis and diabetes. She had been taking prednisone 5 mg daily on a chronic basis but recently had a rheumatoid arthritis flare and the provider increased prednisone to 20 mg daily for 6 weeks. Shortly following the increase in prednisone, blood sugars began to rise.
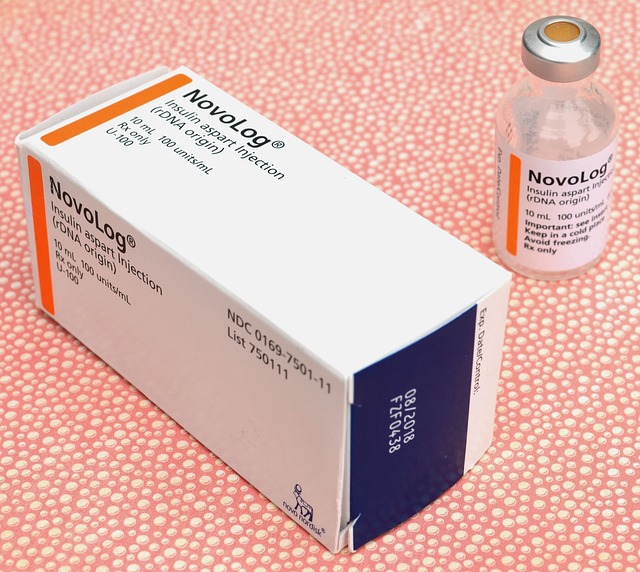
Her insulin regimen before the increase in prednisone was insulin glargine 30 units daily and insulin aspart 8 units before meals. Because of the prednisone increase and the rise in blood sugars that it caused, her glargine is now at 40 units daily and insulin aspart is at 12 units three times daily before meals.
Over the next 3 weeks, the provider is going to try to taper the prednisone back down to 5 mg daily.
- Week 1: Prednisone (podcast) was reduced from 20 mg to 15 mg daily.
- Week 2: Prednisone was further tapered to 10 mg daily.
- Week 3: Prednisone was reduced to 5 mg daily.
This is a great example of how one medication can affect another disease state and the interplay between prednisone and diabetes. As we taper the prednisone, blood sugars are likely to fall and this patient may be at risk for hypoglycemia if they drop too quickly. Hopefully the patient and provider are paying attention to this and follow blood sugars and reduce the insulin dose accordingly.


I would be more specific. What was the glucose BEFORE increasing prednisone and how much did it rise? I MIGHT NOT DO ANYTHING in the short run unless there were LOTS of symptoms (e.g., polyuria). Letting the patient know the glucose can increase and knowing what adjustment to make if there are lots of symptoms makes sense to me. Where is the evidence 3 weeks of higher glucose results in a “worse” outcome?