Medication Review tonight – This medication list is obviously a case of high blood pressure. Amlodipine, clonidine, losartan, metoprolol, as well as torsemide and the tamsulosin have the potential to bring the blood pressure down. It certainly looks like this is a case where would need to monitor blood pressure closely. – As always, please feel free to add anything to the comments following this post.
On the positive side, there isn’t any duplication in the classes of antihypertensives being used, and I don’t see any notorious medications that cause or worsen hypertension.
From the medications, I’m also guessing that this patient has a history of anemia (on Iron supplementation). We need to always assess ongoing use of iron as it can be problematic especially in the elderly (GI side effects, constipating etc.) Here’s a case that I’ve seen too many times on iron supplementation. If the anemia is very significant (or exists), we will need to certainly continually assess the Coumadin use closely as well.
I would suspect this is an elderly patient (but not necessarily) so I would also be looking closely at kidney function. The Macrobid is especially something important I’d be checking out. Plenty of other lab/vitals monitoring to be done as well – just a few to note; electrolytes, kidney function, pulses, CBC, INR, etc.
Assessment of pain would be an important factor as well – this can play a role in contributing to elevated blood pressure. The regimen seems a little bizarre with scheduled Ultram and prn Vicodin (the prn got cut off in the picture).
Why the vitamin E, and cranberry of benefit with Macrobid!?!?
New to the blog? – get something free: 30 medication mistakes that I see in my everyday practice as a clinical pharmacist (6 page PDF I will personally email to you).
Eric Christianson, PharmD, CGP, BCPS

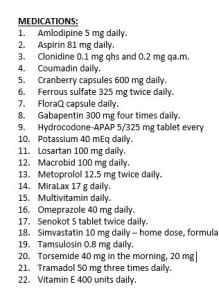

From the meds listed there is a good chance this is also a heart failure patient. Metoprolol tartrate isn’t a great blood pressure drug and there are beta-blockers with better evidence for heart failure. Amlodipine can contribute to peripheral edema (and greater torsemide use). Depending on the patient’s actual situation, I would consider stopping the amlodipine and changing metoprolol to carvedilol. This would maximize the blood pressure benefit with a non-selective beta blocker, give better evidence-based HF treatment, and simplify the overall regimen. By titrating the carvedilol to a maximum tolerated dose (limited by heart rate), it may ultimately be possible to back off of the clonidine as well.
Thoughtful considerations! Thanks
Why do so many patients develop allergic reactions to Amlodopine and Lisinopril?
Andrew,
Excellent pharmacological considerations, Andrew. I also agree that carvedilol will be a better alternative here , however, the lack of Dx, and age, and gender and race information makes any possible clinical pharmacological consideration very inaccurate . Not having the information of age and race will also make difficult to use a proper JNC-8 guideline to consider. However, I agree that carvedilol will be better than metoprolol in any cardiomyopathy. It is also a great assessment to mention amlodipine as a peripheral edema inducer, contributing to dose increase of torsemide, and of course, contributing to adding more medications to the polypharmacy profile of the patient. I do believe that amlodipine should be eliminated (if possible) and that perhaps consequently the gabapentin be discontinued as a result, since it is possible that the amlodipine is also inducing peripheral neuropathy here.
My comment is you know nothing about the patient EXCEPT a list of meds. That leads to the problem of making assumptions. What is needed is a problem list. Are there drugs without an indication? Are there drugs that could be stopped? How about knowing the patient’s age and gender? What is the BP and HR? There are things I would prefer not to use, like clonidine. The patient could also have CAD and needs a beta-blocker to control angina. You can assume has anemia with FeSO4, but you do not know what is the Hb. How long should anyone need iron? NOT FOREVER, that is for sure, to treat Fe deficiency anemia. Giving even 81 mg of aspirin increases the risk of bleeding compared to nothing. Why it that prescribed? Everyone old enough needs aspirin or did the patient have a TIA, stroke, or have CAD? Is the omeprazole for an ulcer, GERD, or to be gastroprotective? Was the patient in the hospital at some point and given omeprazole for stress ulcer prophylaxis and it was never stopped? If the patient has not responded to FeSO4, then one should think that giving omeprazole (especially at a higher dose) could be related to decrease iron absorption. There are LIMITED data to show this is a clinically important issue (Am J Ther 2012; 19: 185). If the Hb is not increasing, then is it the wrong diagnosis (e.g., B-12 deficency that may happen as a result of long term PPI ingestion). What is gabapentin for? Plenty of patients getting this for some pain related issue and it does not work and hence tramadol started and NOW is comfortable: stop gabapentin?). There are far too many unknowns to do more than speculate what is right or wrong about this list of medications.
Thanks for the comment Bill! All very relevant questions – thanks for raising them, it really gives a sense of what all goes into the clinical thought process. My goal with the med lists are to draw some of those questions out that clinicians might not think about. Your background I’m sure is much different than mine and its great to get ideas and questions to consider from other caring professionals. My posts are indeed speculations based upon what I’ve seen in my practice – my goal is not to find a right or wrong answer, but to try to teach the process. Thanks again for the comment – take care, Eric
Excellent Bill! Great assessment! I think that the SOAP platform should be utilized to initiate and conclude a good clinical pharmacy assessment. Many parameters and variables are missing here to conclude anything meaningful from the case. Pharmacoclinicians should not make assumptions, as we can only work with the right empirical tools to make determinations with the minimum necessary empirical data. Without basic demographics (age, gender, race) and no Dx information, this makes impossible to speculate anything. A drug list only tells nothing about a patient condition, and also tells the clinical pharmacist, that the patient drug profile is not all is needed to make clinical determinations of therapies, since it only tells about 20-30% or less of the whole clinical case .
Hey Eric,
Thanks again for all your posts really helpful. My question is regarding beta blockers. If patient is on propranolol for esophageal varices or thyroid storm or migraine or essential tremors can they also be on metoprolol or carvedilol for HF indication? I know in your CGP webinar review you said probably not but how would you approach this with a physician when it comes to esophageal varices as one of the examples that I commonly see? I would also appreciate so feed back from other pharmacist bloggers.
Thank you in advance
In the majority of situations I would probably like to see them off the duplicate therapy. If propranolol is used for a symptomatic treatment (i.e. tremor or migraine) it might be possible that a non-selective does provide some benefit? Just a couple thoughts… PS thanks for checking out the webinar 🙂 – hope you found it useful!