A computerized Drug Interactions checker can sometimes go way overboard leading to these constant alerts that aren’t taken seriously. As a pharmacist, nurse or prescriber – we need better programs to help identify interactions, but more importantly we need to develop the critical thinking skills to know how and when to address these alerts – i.e. What’s Relevant?
I recently saw a drug interaction fax sent to the doctor about the risk of hyperkalemia of potassium and Lisinopril (both low doses). The risk of this interaction was “severe” according to the computer report. So is this really severe and should a prescriber be alerted?
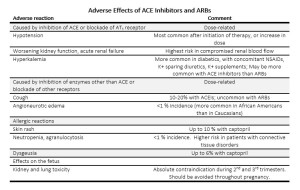
If there it was an unusually high dose of either one of these, I could understand a heightened awareness, but there are other avenues to investigate this. They were also on Lasix (furosemide) and had a history of CHF. I’m a solution oriented individual, so instead of using the time to send that fax and have the doctor sign it (a fact they will know), maybe call and ask the clinic for the most recent potassium level or if lab work is planned in the near future. Another option would be to ask the patient if lab work is planned(which they may or may not know what lab work is planned). The doctor who had been practicing medicine for 10+ years (I would assume was insulted) refused to sign the fax. Everyone dispensing or prescribing should know this fact. Don’t get me wrong, dangerous potassium levels can result and monitoring is essential. ACE Inhibitors raise potassium, and so do potassium supplements. In my mind this would be similar to alerting someone that adding Aspirin to Plavix (clopidogrel) can increase bleed risk. If you do feel that you need to remind a prescriber about this “interaction”, it might be appropriate to tell your patients they should see a different provider 🙂 – Kidding of course… both examples should be common knowledge. This potassium interaction is monitored by checking lab work. In my opinion, it is simple things like this can really damage credibility amongst other healthcare professionals. Not only that, when there is something potentially life threatening or potentially harmful is your voice going to be listened to after potentially sending meaningless information for the prescriber to address? What do you think?
Here’s another post on trying to determine what drug interactions are relevant.
Absolutely free – 6 page PDF on 30 medication mistakes you should be aware of. I created the content based on my real life experiences as a clinical pharmacist – please Click Here to check it out!



Agree, I work at family health team, and I am constantly asked why pharmacists keep sending useless info like this, but ignore more important issues, or if they identify an issues, then why there are no suggestions. E.g . This eye drop is on back order, they want to know what is in stock, -give suggestions.
Would abruptly stopping and ACE inhibitor contribute to hypokalemia?
With this patient being on Lasix, I likely would recommend a follow up potassium level be checked if the ACE was discontinued.
How soon after stopping an ACE would you recommend getting a Potassium level?
Going to depend on history, how high the level, if other identifiable cause etc. If severe/life threatening, obviously immediately.
I had a same situation. And, as suggested I requested for a recent K level. The physician did not like that either. Here, I thought I should have just sent a fax indicating the interaction and sent the patient back to clinic with a complaint that the rx has withheld potassium order. Would you think that may have caught the attention of someone at the clinic?