A 93 year old female was diagnosed with a new onset DVT. Her past medical history includes hypertension, hyperlipidemia, osteoarthritis, osteoporosis, constipation, GERD, erosive esophagitis, peptic ulcer disease, and hypothyroidism. Her current medication list includes:
- Lisinopril
- Hydrochlorothiazide
- Simvastatin
- Acetaminophen as needed
- Raloxifene
- Ranitidine
- Levothyroxine
- Omeprazole
- Aspirin
- Vitamin D
- Calcium
- Senna
- Miralax
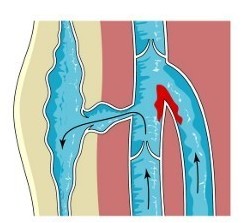
One of the greatest challenges with polypharmacy is to not be overwhelmed by looking at the medication list when new problems arise. So is this a case of drug induced DVT? In this case, the DVT could have been provoked or exacerbated by the raloxifene. Other medical considerations like immobility should be assessed as well. The risks following the new onset DVT would likely outweigh any potential benefit from continuing raloxifene in a 93 year old patient. We would need to assess osteoporosis risk and if other therapy should be continued, but a bisphosphonate would not be a great alternative either given the, erosive esophagitis, GERD, PUD history.
For treatment of the DVT, She was placed on rivaroxaban. A quick point about the rivaroxaban: this will greatly increase our patients risk of bleeding, especially important with this patient’s past medical history of peptic ulcer disease. Monitoring for GI bleeding will be of high importance.
Looking for more case scenarios and clinical pearls? Check out an Amazon best seller!


I would question the appropriateness of rivaroxaban in this patient, especially given the history of PUD.
cannot see any indication for aspirin (primary prevention?)-stopping this if not indicated could reduce risk of gi issues on continuing with rivaroxaban. Also depending on fracture risk could bypass gi route and have denosumab inj if no other contraindications and calcium and vit d replete