A 78 year old male was found driving around in his car making abnormal turns and proceeded to drive to a parking lot where he was driving in circles. He presents to the ER with primary symptoms of confusion and cognitive decline. Vital signs were fairly normal with a significantly lower pulse noted.
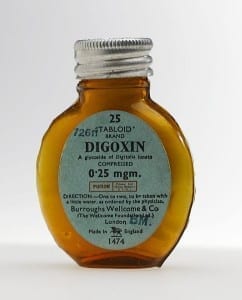
Upon review of his medication list, it was noted that he was on Digoxin 375 mcg daily. This is a high dose for a middle aged individual. Remember that this patient is 78!
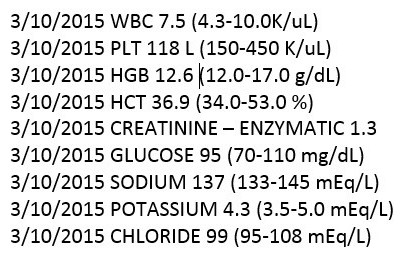
Upon checking a digoxin level, it was quickly confirmed that he had digoxin toxicity. His level was 7.58! Usual upper limit of normal is considered to be about 2. This is the highest digoxin level I’ve ever seen. The part that amazed me was that he really wasn’t displaying many classic digoxin toxicity symptoms. If you ever see an elderly individual on 250 mcg daily or above, this should be an immediate alert in your head to monitor closely for digoxin toxicity. The dosing of 375 mcg daily in this case would be of high concern to (at a minimum) monitor. This gentleman did have some renal insufficiency as well. Always remember that digoxin is cleared by the kidney!
I would also add that with this gentleman’s confusion, it would be nice to try to dig into the patient history to identify if he has had cognitive trouble before digoxin toxicity as well. This is a very high digoxin level and I will never know, but suspect that this patient may have inadvertently been taking more than one tablet per day. What’s the highest digoxin level you’ve seen?
Want more clinical pharmacy pearls? Do you want them for free? Click here to check out 30 medication mistakes I commonly see in my practice as a clinical pharmacist!


Love your posts. Always a treat.
Thanks Scott!
Describing a Dig level without discussing the timing of the test (with regard to when the patient took their last dose is useless). I’m also disappointed that after you suspect dig toxicity you don’t mention checking for drug interactions or potassium levels. I don’t think this is dig toxicity (very rare without nausea/vomiting) but if it was was he administered digibind? I consider this either inadequate clinical pharmacy support or a very incomplete picture…
Appreciate the comment, it is a challenge to put down every possible factor in a case and yes I concur those are important points to raise. I actually came across this level after they were off the digoxin (reviewing previous records), and I likely suspect it was digoxin toxicity due to the fact that multiple levels were drawn and showed a still elevated, but downward trend after stopping the drug. I do not remember seeing either way if digibind was administered. My speculation is that it was. Take care, Eric
I always learn so much from your posts. You have a great way of explaining things that sticks in my head. I can’t thank you enough for what you do Eric!!
Thanks Sherrie, appreciate the comment!
The dose is high given what we know about the patient. It seems to me to be higher than I would expect in 78 year old with Cr 1.3, so more information is needed I saw a few patients with higher serum concentrations.
i would say this is very likely digoxin toxicity if the patient got better when digoxin was stopped. The definition of what serum concentration = toxicity was based upon the concentration identified AFTER digoxin was stopped and then what happened to the patient in recovery. IF there was no change, then the patient did not have digoxin toxicity. the “classic” NEJM article defining 2 ng/ml as the threshold of toxicity actually had a preliminary results publication in J Clin Invest with fewer patients and the average level was lower than 2. There are studies showing mean levels <2 ng/ml defining toxicity. The real issue is whether the patient improves (or dies of arrhythmia).
An evaluation of non-cardiac toxicity of digitalis toxicity was reported 45 years ago after digoxin tablets were mismanufactured and contained 0.2 mg of DIGITOXIN and 0.05 mg of digoxin (BMJ 1970; 3: 737). The most common non-cardiac toxicity was fatigue and visual changes (95% for both). The visual changes were BLURRING of vision and not changes in red-green perception or halos around lights. Psychiatric manifestations, including confusion, "organic brain syndrome" was common (65%) and more common than vomiting (40%).
It is important to assess K, but also Mg, Ca, and HCO3 since hypo-Mg, hyper-Ca, and alkalosis can potentate toxicity. Other meds can reduce clearance, and knowing those would also add to the case. It is not stunning to have levels <2 ng/ml and have CLEAR digoxin toxicity. The levels are mostly CONFIRMATORY of what you can observe: if level 7.5 it MUST be toxicity and if 1.5 it must not be toxicity. That is CLEARLY wrong. TWO quick anecdotes. A man who was 85 years old walked into the clinic and said he did not feel good. He had CAP and like lots of old and sick people he got AF in the hospital and was given digoxin. He went from being completely alert to being unresponsive over a few days. His level was 1.5 ng/ml and electrolytes were normal. The VR did not come down much (not a shock when sick either) and metoprolol was added. VR came down and it took some talking but the intern finally DC'ed digoxin. Two days later the patient was WIDE WAKE. Second patient was in his 70s transferred for "terminal care". He looked like he had been in a concentration camp and a million dollar work up revealed NOTHING. The attending and I said to STOP digoxin and in a few days the patient WOKE UP and could not stop eating.
Digoxin toxicity can be VERY subtle. neuropsych issues are COMMON and often not considered as part of digoxin toxicity. Although it would be great to know the timing of when blood drawn and when dose was taken, it seems unlikely to me that is a huge issue in this case. It would be interesting to know if a second serum concentration was done and if it seems consistent with the first one.