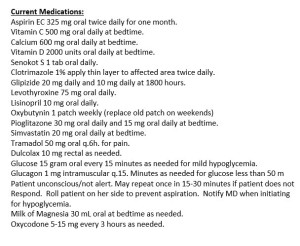
Pretty extensive med list, and I’m going to pick out three points that need to be investigated – It’s really hard to limit it to three, but that gives you all an opportunity to identify other potential problems!
1. They have orders for management of hypoglycemia here, and they are on a very steep dose of glipizide – it’s pretty obvious to me that we need to monitor blood sugars very closely! On Actos (pioglitazone) as well which is split up into two doses. Usually given once daily, but would need to investigate that further as well.
2. Oxybutynin patch is usually dosed twice weekly – certainly need to address this and make sure that is correct, beneficial, and tolerable for the patient.
3. Appears to be a probable rehab patient with the Aspirin dosed twice daily for one month. One thing I’ve come across several times is to make sure that anticoagulation/antiplatelet therapy get addressed long term versus short term. In this case, there is no noted order to continue Aspirin for CV prophylaxis, and they are likely a candidate long term being on the statin with diabetes meds. GI and bleeding risk history certainly needs to be assessed as well before continuing long term antiplatelet therapy.
As always – comments/suggestions are encouraged!
For strategies to help minimize polypharmacy, subscribers have unlimited and free access to a webinar of the 10 Commandments of Polypharmacy – Please sign up! More content is in the works as well! Simply subscribe on the upper right hand side of the page (or down at the bottom of the page for mobile users).



While the comment on the dosing schedule for Actos and Oxybutynin are valid we need keep in mind that manufacturers recommended dosing schedules are not a bible and we are treating people and need look at their individual response to a varied schedule. If its not broken don’t try to fix it,
Excellent comment – I can feel a new post coming on! – Thanks for your input
Agree generally but knowledge of PD/PK parameters should inform as well. Makes zero sense to dose a med that takes months to reach full efficacy such as pioglitazone BID. More likely to decrease compliance, pill burden. Would be like dosing levothyroxine BID. I’m not bothered by glipizide dose–suggests SMBG pattern of daytime elevations vs fasting. Lows with this med almost always associated with not eating carb consistent diet. Like an insulin order, can always add hold parameters for no food intake (if good nurses can specify carb intake).
Opioid use here is suboptimal. If tramadol is scheduled here to leverage noradrenergic properties would convert to another neuropathic pain med such as gabapentin/pregabalin or duloxetine. Would eliminate dual opioids. If really needing that much opiate, need to give long acting to avoid peaks/troughs. Lots of prn laxatives. Would be sure to titrate senna or add PEG given large opioid requirements. Also consider effect of oxybutynin on constipation as it is anticholinergic.
I would question using either of the two short term opioids when either tramadol or oxycodone could be substituted with a longer duration opioid ( depending on pain score).
Although it’s not the top priority I would ask about the Vit D dose. Seems high unless there is a reason. Too much can cause big problems. Add her diagnosis list and then I will most likely back down.
Metformin???