If you haven’t subscribed yet for future updates and access to more free clinical medication content, please Click Here to do so!
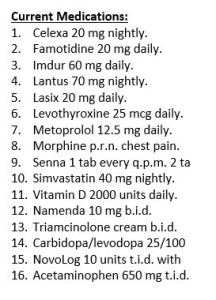
I’m going to cover a couple points tonight, and let you guys help with anything else you’d be concerned about by looking at the med list!
The morphine dose certainly needs to be clarified, and along with that we might as well ask how frequently it is used for chest pain. Along with the potential for chest pain and cardiac type medications, it is pretty suspicious that this patient is not on an antiplatelet of any kind? Maybe bleeding risk history? Frequent falls potentially Parkinson’s with Sinemet Rx?
The other point I will mention is that this patient is on a fairly substantial dose of insulin – so we certainly need to pay close attention to blood sugars and any abnormal symptoms as this patient likely has dementia being on the Namenda. Hypoglycemia identification can often be a challenge in dementia.
Definitely a couple other things to monitor and point out here…thanks for your help in advance!



He could have a rash? I know brilliant contribution right?
In all honesty with all the other meds, it didn’t even cross my mind…its a really good point that assessing what they are using it for and if they are still using it matters. Always important to look at drug adverse effects and contribution to skin/itch/rash issues – I’ve got a case on that coming up in the next few weeks!
At only 20 mg of famotidine one would have to wonder why the patient is not on at least low dose aspiring therapy as any bleed cannot be significant. I would also question the use of morphine for chest pain versus SL nitroglycerin for acute pain not prevented by the Imdur. Acetaminophen would be a suspected cause for any rash and offering only minor analgesia and no anti-inflammatory activity questionable as to its intended use,
Few concerns I have as a pharmacist:
1. Is this a polypharmacy patient? How compliant are they on their medications?
2. Is it Parkinson’s disease or is the patient hypoglycemic? What’s their most recent FBG and A1c levels? Also a concern with being on a fairly high dose of Lantus and metoprolol (albeit LD metoprolol). Maybe reduce Lantus dose and NovoLog dose?
3. What’s their most recent vital signs and CMP labs? Lipid panel? Thyroid lab values? Based on that, there may be some meds that can either be discontinued or monitored closely.
4. Similar with Leo’s comment, why not use SL NTG instead of morphine?
5. What about the OTC meds? Why are they on APAP? Senna? Is it PRN?
6. Why not put them on metformin instead? Are there any contraindications for them being on metformin therapy?
7. What’s their HPI, Past Medical/Surgical History, Family History, Social History, objective findings?
More questions than answers for me. Once I have subjective and objective findings, *maybe* we can reduce their medications from 16 to maybe (dare I say) 8 medications? Less medications, improved compliance, decreased unnecessary healthcare spending, and improved overall quality of life? Works for me!
Seems a very low dose of levothyroxine, does patient have heart issues?
There are drug routes and frequencies missing. Where is the past medical history, past surgical history history, allergies, etc.? Maybe it’s just an incomplete med list. Thank you for this exercise Eric, goodnight.