88 y/o with a history of depressive type symptoms was placed on an antidepressant to manage symptoms shortly after admission to a long term care facility.
This particular patient was trialed on Zoloft (sertraline) and then transitioned to Cymbalta (duloxetine), neither of which made a significant difference in symptoms. This patient continued to have ongoing symptoms of depression despite antidepressant therapy.
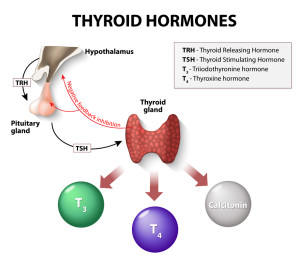
Hypothyorid symptoms can often overlap/mimic signs of depression and this is a scenario I’ve seen play out several times. What was of note, was that the patient was on chronic amiodarone for an arrhythmia. Amiodarone has many unique side effects one of which is it can affect thyroid function. It was requested that a TSH be checked to monitor for this unique side effect of amiodarone. TSH labwork was done and elevated at about 30 indicating hypothyroidism – normal range is approximately 0.5-6 depending upon the lab. Synthroid was initiated and the symptoms of “depression” started to improve allowing for discontinuation of the Cymbalta (duloxetine).
Please take advantage of a free 6 page PDF – 30 medication mistakes every healthcare professional should know! A resource I created based upon my experience as a clinical pharmacist.



I would think that the interaction between different drugs therapies and idiopathic problems would be set up on a physician carried iPad I can’t believe that medicine is not into the Star Trek age where a lot of geeks have a gaming apps that are more advanced than hospital apps that’s why there are so many medical errors. Maybe apple programmers should recant hospital and medical programs
Excellent information! Very useful clinical pearl!
Excellent information..
So due to following your blog, I had to look up if you had a blog post on this situation, because we had a similar situation inpatient where a patient’s TSH was 9, and currently taking amiodarone. My question is therefore, is the appropriate response to treat the hypothyroidism then? Or only if the patient is symptomatic? Thanks in advance!
It’s controversial 🙂 I have seen both done in practice. My sense would be to continue to monitor in most situations. I would engage the cardiologist or whoever is prescribing the amiodarone and see how long they are going to be on it and if it is necessary and assess other alternatives. If we can get rid of the amiodarone, we can likely get rid of the subclinical hypothyroidism if we truly know that it is from the amiodarone. It is a tough one and I’m not aware of a right answer on this one.