Polypharmacy is a horrible problem in geriatrics. I came across this medication list, and just wanted to give you a brief idea of some of the thoughts that go through a clinical pharmacist’s head. Scary I know, but just stay with me, as you will most likely see something at the end of this post that you’ve never seen before. I’ve spoken with a couple people who’ve been in the business a long time, and they can’t recall a medication list quite like this either.
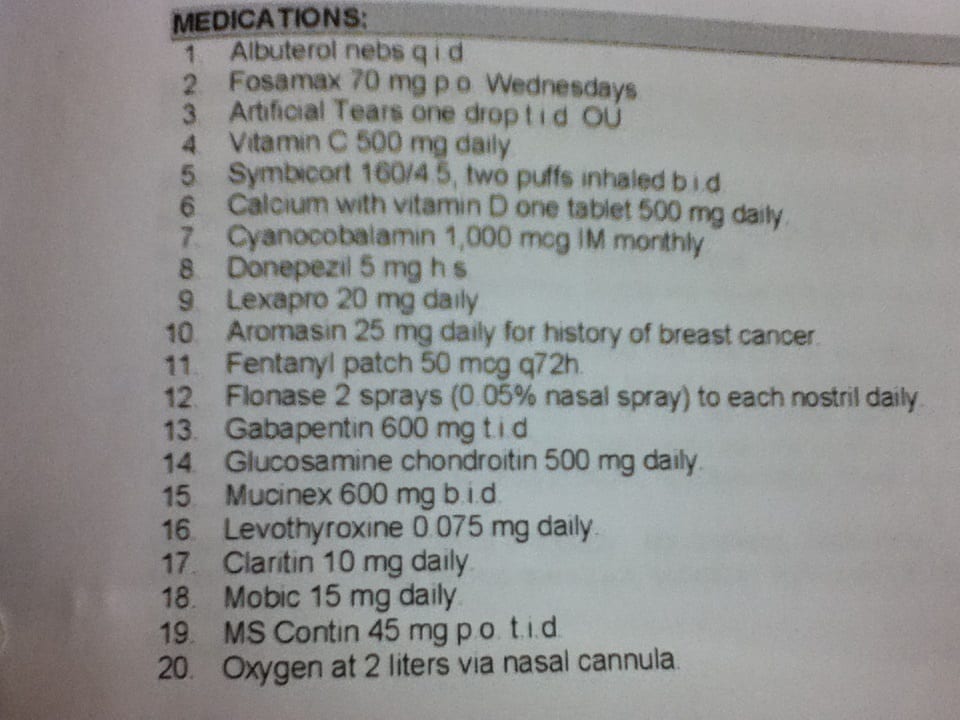
Certainly you need more information than a medication list to determine appropriateness of each medication that a patient is on. However, you can begin to form ideas in what you might change about a patient’s medications, identify potential problems, and get your mindset geared as to what to try to look for when reviewing a medication list. As I was reading, this particular patient was on about 20 meds.
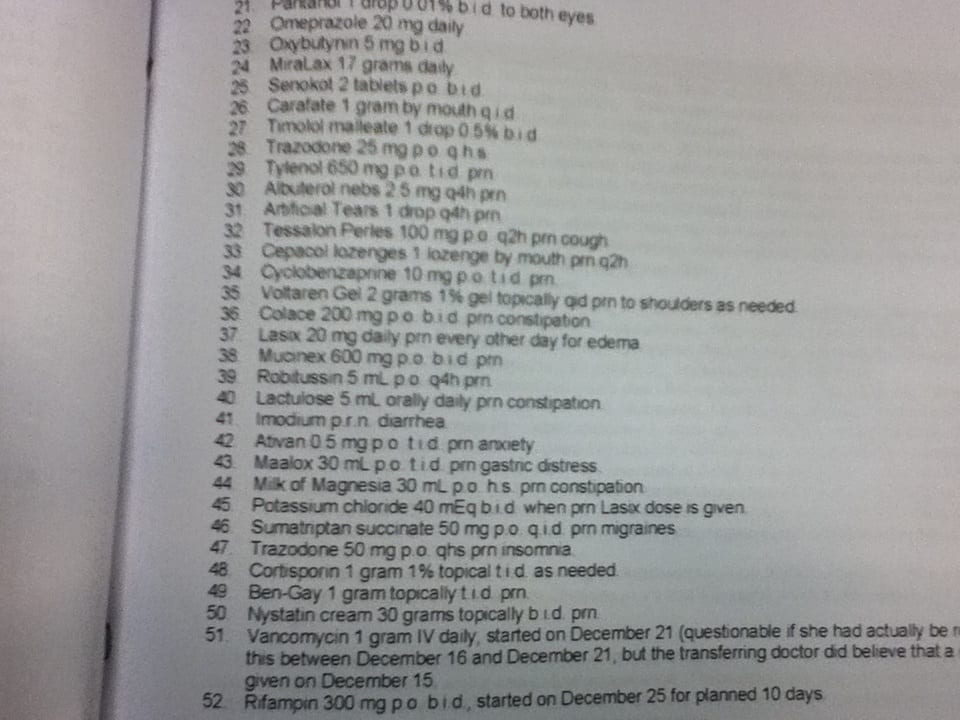
In going through this medication list, I look at a few respiratory medications and oxygen, obviously this is a patient with some serious respiratory issues, so we need to be mindful of that. All the doses look low to moderate with the exception of the opioids and gabapentin which is at a moderate dose, so I would certainly make sure to keep an eye out for side effects of gabapentin as well as kidney function as gabapentin is eliminated through the kidney. This patient is certainly getting a significant amount of opioid with no noted constipation medication – so we need to watch out for that. They obviously have some serious pain management issues and ideally it would be nice to convert them from 2 long acting opioids to one (Fentanyl and MS Contin) at some point in time. This patient doesn’t have a prn opioid for breakthrough pain either…kind of bizarre for someone on that high of a dose of opioids. Donepezil could potentially be increased to maximize the potential benefit depending upon GI status and if it hasn’t been tried in the past etc. They obviously have some sinus and/or allergy issues on Mucinex, Claritin, Flonase – maybe we could try to wean those down at some point if symptoms are well controlled. Some other thoughts to try to minimize this patient’s medication load would be to look at vitamin C and what that is being used for, as well as the glucosamine as obviously there may not be much pain benefit if using for osteoarthritis (remember the large amount of opioids and on Mobic. They are also on an NSAID (Mobic) so we will need to do some lab monitoring there as well. A TSH needs to be monitored on Synthroid. Those are just some of the ideas that went through my head by simply looking at the medication list without yet looking into symptoms/assessment/H&P/vitals etc. There really wasn’t anything too crazy about this case that I hadn’t seen before. If you are a patient, you are probably thinking that this is a ton of medications. If you are in healthcare and work in geriatrics, this is probably nothing you haven’t seen before. I deal with patients on 10, 20, and sometimes even 30+ medications on a daily basis. Helping physicians and nurses identify medication related problems is what I do, and from the above, you can get a small glimpse of that. What separated this case from others I’ve seen is that I flipped to the next page in the H&P and saw this:
I was speechless, and pray that I will never see a medication list like this again!
Thanks for reading! Please subscribe to the blog as I’m giving away a 6 page PDF on 30 medication mistakes I see in my practice as a clinical pharmacist.



Go to any care home and you will see list like this. The worst script was when i was agency & was for digoxin for a resident with a pacer and he had been given it for months
it’s not unsual read this article from PUBMED http://www.ncbi.nlm.nih.gov/pubmed/7439229
Unbelievable. I’ve never seen anything like that before
I hope you changed something about it. Would be a good project and needs the collaboration of a good and willing physician to wean some of the meds out!
It’s a work in progress!
This is quite a list. Unusual ? Not so. In Medicaid we see too often the excessive medications being dispersed Not uncommon to see 20 , 30. Or more than 50. Several issues in Medicaid. Possible Diversion. Possible multiple prescribers. Possible sharing with family or friends The low to no cost copayment , offers financial opportunity for diversion and collusion. Phantom prescriptions may also be part of the concern. Especially due to the member not having Rx claims awareness being a sentinel event for there awareness. My experience leads suspicion to Rx’s greater than 10 per month based on disease diagnosis.
Auditing and monthly plan director awareness is needed to stem the issues. Tom
Just a thought. Have you ever seen the medication list of a heart and/or lung transplant patient? What about kidney or liver transplant? 20 to 25 medications are not so far beyond imagination.
I’ve seen a handful of transplant patients and it can get pretty complicated, pretty fast! 20-25 meds definitely not out of the question
What was outstanding is not merely the quantity of medications but the redundancy!! Trazodone and Lexapro?!? Then Carafate -when was the opportunity to separate those dosages from everything else? This looks like a classic example of old meds being replaced with new therapies and the old not being DC’d. I didn’t look at the rest of the sheet because I’ve seen it often as well.
When I was doing MTM, I once had a patient taking several hundred tablets weekly with duplicate therapies. This is where we can really have a beneficial impact for the MD’s!!! When we do our reviews, we truly help them prevent med errors and help save patients lives!
Thanks for the comment!
Eric
This is lazy prescribing and is meant to let the nurses handle more than they are educated to handle.
Lots of PRN, with several PRNs for an indication. Is the nurse to give all of the PRN constipation meds – or just one, or two – when the resident has constipation?
This is a way to avoid having nursing call the prescriber when a “common problem” appears, which has the potential to hide negative effects that the prescriber should be notified of to think about whether something is going awry.
Any updates on what happened with this one? Would love to follow on a case! I see obvious duplications of albuterols, artificial tears, Mucinex, trazodone – two different doses <- or is it that in a nursing home they have prescribe two orders if they really mean 25-50mg HS PRN? <- I think they have to do that in the hospital setting for pain meds. Is the nurse supposed to choose which laxative to use? How are you approaching constipation d/t narcotics these days? In school it's always senna and colace, I've been following FreeCE's OTC certification – he seems to be against senna+collace camp.